By Evangeline T. Capuno
Tuberculosis (TB) became the talk of the country in the 1940s when then president Manuel L. Quezon was infected with the ancient scourge. He was in exile – because of World War II – when he died of it in Saranac Lake, New York.
In the 1990s, TB again struck another Filipino celebrity in the person of Rene Requiestas. The comedian and television personality – who was known for his sidekick roles alongside other comedy actors – died as a result of the disease in 1993.
Despite advanced knowledge in science and recent discovery of sophisticated drug regimes, the disease has continued its deadly progression. “Tuberculosis is perhaps the greatest killer of all time,” wrote Dr. Frank Ryan, author of Tuberculosis: The Greatest Story Never Told. “Tuberculosis rose slowly, silently, seeping into the homes of millions, like an ageless miasma. Once arrived, TB stayed (and became) a stealthy predator.”
The “predator” is now out of control in many parts of the world, including the Philippines. “Each person with active TB can spread the disease to 10 other Filipinos each year,” reminds Dr. Willie T. Ong, an internist-cardiologist who writes a regular column for a national daily.
Ancient scourge
The tenacious MTB has preyed on people since antiquity. TB-induced skeletal deformities point to the disease’s existence as early as 8000 BC. Unmistakable signs of tubercular bone decay were found in the skeletons of Egyptian mummies as long ago as 2400 BC.
“Year after year, century after century, it tightened its relentless grip, worsening with wars and famines that reduced people’s resistance, infecting virtually everyone but inexplicably sparing some while destroying others,” wrote Dr. Frank in his book.
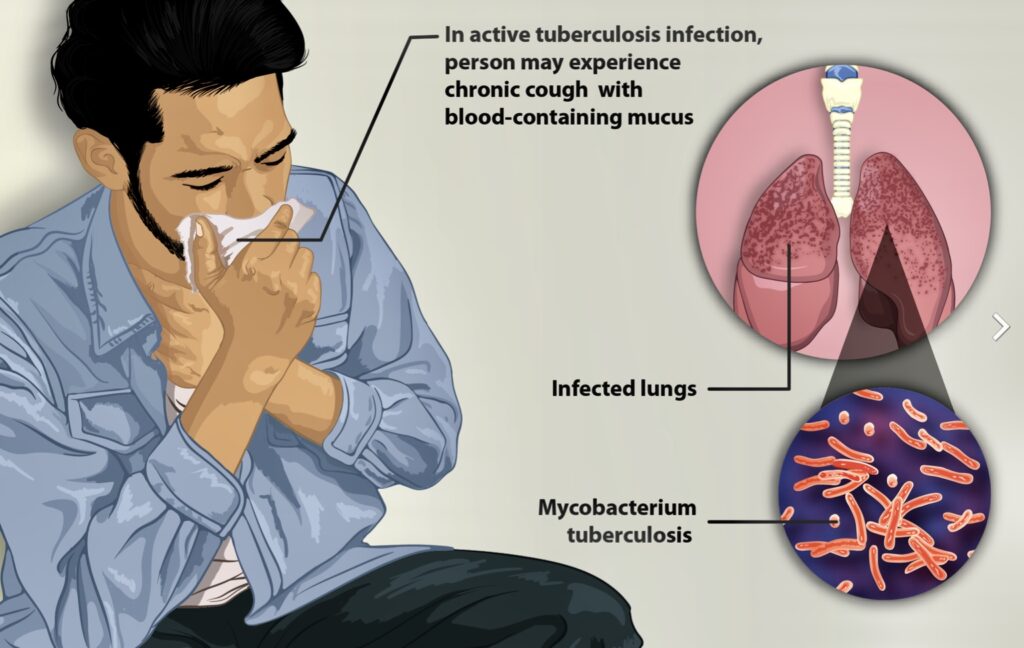
TB infection is transmitted almost entirely by the aerial route. “TB is a bacterial infection that can spread through the air,” the TB Alliance explained. “It is most often found in the lungs, but can exist in any organ of your body.”
When people with TB coughs or sneezes, they can transmit so-called “active” TB. “Many people are also infected with an inactive form of TB, known as latent TB,” the TB Alliance said.
TB bacteria
The MTB’s unique cell wall, which has a waxy coating primarily composed of mycolic acids, allows the bacillus to lie dormant for years. “The body’s immune system may restrain the disease,” the TB Alliance said, “but it does not destroy it. While some people with this latent infection will never develop active TB, five to 10% of carriers will become sick in their lifetime.”
A long time ago, TB was already considered the world’s deadliest disease. But it all changed when 21-year-old “Patricia” with progressive, far-advanced pulmonary TB received the first injection of streptomycin in 1944. She improved dramatically during the ensuing five months and was discharged in 1947.
“Patricia” was evaluated in 1954 and found to be healthy and the happy mother of three children. “This injection began the age of modern anti-TB treatment and led – until recently – to dramatic reductions in TB in industrialized countries,” the World Health Organization (WHO) says.
Other anti-TB drugs are thiacetazone (first introduced in 1946), isoniazid and pyrazinamide (both first tried in 1952), and ethambutol (used for the first time in 1961). The most recent one, rifampicin, was released in 1966.
Correct treatment
According to Dr. Ong, the treatment for TB is a bit more complicated compared to ordinary infections “since it will take approximately 6 months to completely eradicate the bacteria.” In cases where the infection is serious, it may take about 9 months of treatment.
Only a doctor can give a person with TB a correct treatment. “Never self-medicate,” Dr. Ong reminds. “This is the worst thing you can do. It will only strengthen the bacteria inside you and make you resistant in one tablet.”
Dr. Ong suggests that those who are undergoing treatment should stay at home during the first 3 weeks of treatment. “Don’t go to school, work or come in close contact with people,” he says. “Your saliva and phlegm can infect others.”
He also recommends that they wear a face mask during the first 3 weeks of treatment. “Cover your mouth with a tissue when you cough, sneeze or laugh too hard,” Dr. Ong suggests. “Then throw the tissue away in a sealed container.”
As a sort of reminder, all TB medications must be taken one hour before meals. “It is ideal not to break the dose of the drug,” Dr. Ong reminds. The patient needs to see his doctor to undergo blood tests to check for possible liver side effects of the drugs taken.
Side effects aren’t common but some TB medicines can occasionally be harmful to the liver, he says. In addition, the color of the urine will change from yellow to orange. But don’t worry; the change of color is “a normal reaction to the treatment course.”
Dr. Ong suggests that you need to consult your doctor once you experience any of the following: nausea, vomiting, loss of appetites, yellowing of the skin, or fever of more than three days.
The most important thing: “Complete the 6- to 9-month course of your medicines,” Dr. Ong urges. “Do not stop your medicines without your doctor’s permission. Doing so will cause the TB bacteria to mutate and come back in a stronger and more virulent form.”
Multidrug resistant TB
But like a phoenix that rises from ashes, TB has staged a comeback – in a deadlier and more complicated form. In 2017, the United Nations health agency estimated that 10 million people became sick with TB, with more than half a million cases being multidrug-resistant (MDR-TB).
“There is growing resistance to available drugs, which means the disease is becoming more deadly and difficult to treat,” the TB Alliance pointed out.
MDR-TB develops when the long, complex, decades-old TB drug regimen is improperly administered, or when people with TB stop taking their medicines before the disease has been fully eradicated from their body. “Once a drug-resistant strain has developed, it can be transmitted directly to others just like drug-susceptible TB,” the TB Alliance said.
About one in 5 cases of MDR-TB around the world go untreated. “Without action, there will be more MDR-TB,” the TB Alliance cautioned. “As a result, the cost of fighting TB will continue to rise.”
Bedaquiline
Meanwhile, Médecins Sans Frontières (MSF) or Doctors Without Borders urged the American pharmaceutical corporation, Johnson & Johnson (&J), to publicly announce it will not enforce any “secondary” patents for the drug bedaquiline in any country with a high burden of TB and “withdraw and abandon all pending secondary patent applications for this critical drug everywhere.”
Bedaquiline tablets are now the backbone of TB treatment regimens, recommended by the United Nations health agency for a far-improved, shorter, better-tolerated and more-effective treatment for people affected by drug-resistant TB. The current recommended treatment, containing bedaquiline, is all oral, 6 months long and can achieve cure rates as high as 89%. This is a vast improvement over the older treatments that had to be administered for 18 months and included daily painful injections.
Causes of return
Poverty has been cited as the major reason for the resurgence of TB. “Overcrowded, impoverished dwellings are its breeding ground, and TB thrives on immune systems weakened by other chronic infections and by malnutrition,” said The Stop TB Initiative Report. “Even before the cause of TB was discovered in 1822, thus paving the way to effective drug treatments, the rates of disease were falling in many developed countries because of an improvement in peoples’ standard of living.”
A significant cause of the dramatic rise in TB cases from the mid-1980s onwards is the human immunodeficiency virus (HIV), the microorganism that causes AIDS. “TB and HIV/AIDS are a deadly duo,” the TB Alliance stated. “HIV weakens people’s immune systems, allowing TB to flourish.”
The fight against TB is far from over. “We need short, safe, and user-friendly drug regimens to help improve treatment compliance, prevent drug resistance, and save lives,” the TB Alliance said. “New drugs must be adopted and used for those in need. We also need simple point of care diagnostics and a better vaccine that can help us finally rid the world of TB for good.” – ###
Photo captions:
1) Infected person (Source: Wikipedia)
2) Tuberculosis (Source: biomedcentral.com)
3) Scanning electron micrograph of TB bacteria (Source: Wikipedia)