By Evangeline T. Capuno
“Cervical Cancer is highly preventable and treatable,” World Health Organization (WHO) chief Tedros Adhanom Ghebreyesus recently tweeted, saying “it could be the first cancer ever to be eliminated.”
Cervical cancer is largely preventable through both vaccination and screening for precursor lesions, with appropriate follow up and treatment, according to the International Agency for Research on Cancer (IARC), an intergovernmental agency under the WHO umbrella.
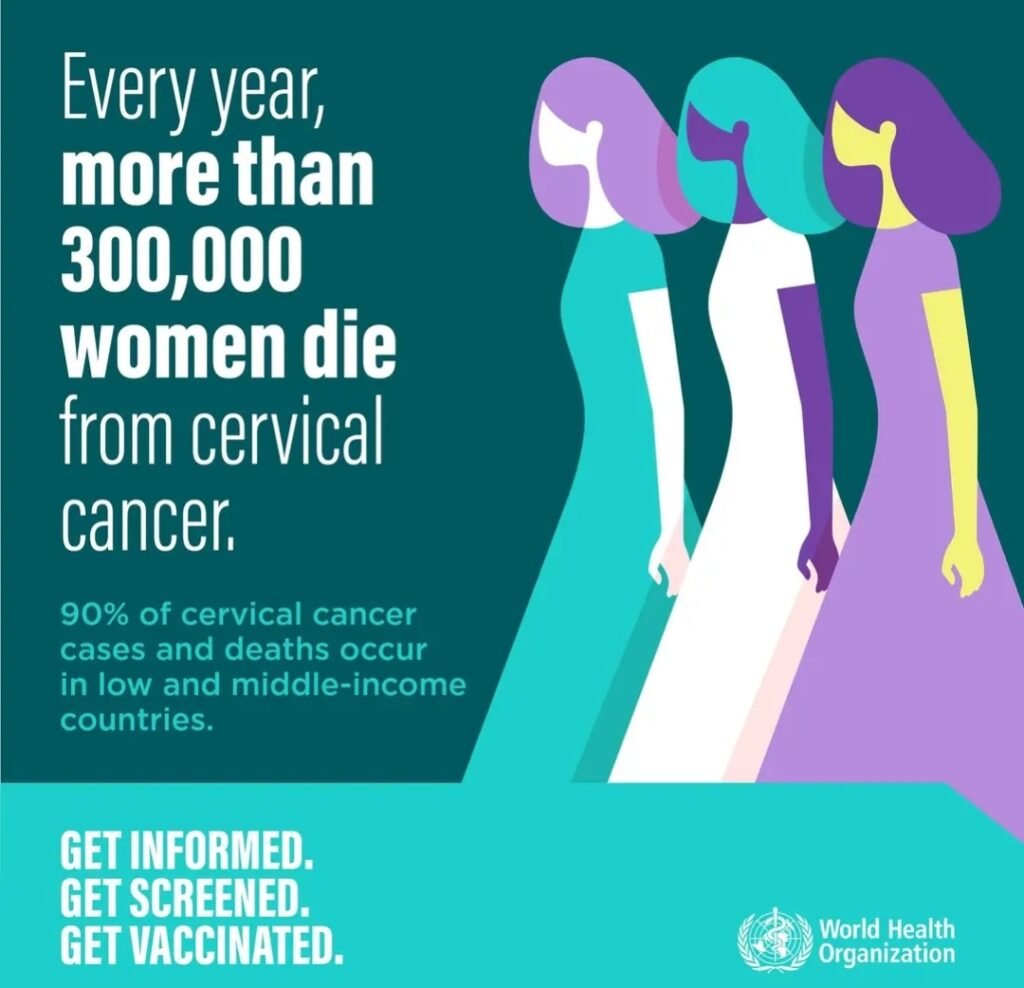
Cervical cancer is also the second most common cancer type for women, with the highest incidence and mortality rates, generally impacting low Human Development Index countries.
The Geneva-based WHO ranks cervical cancer as the fourth most common cancer in women globally. In 2020 alone, an estimated 604,000 women were diagnosed with cervical cancer, 342,000 of whom died from the disease.
Last December, the Manila Standard reported that “11 women die of cervical cancer every day, meaning one Filipina dies from the disease every two hours.” This makes it the second most frequent cancer among Filipino women, particularly among those between 15 and 44 years of age.
“Annually, there are nearly 8,000 new cases and more than 4,000 deaths due to cervical cancer in the country,” Manila Standard reported. “These numbers are projected to increase, with more families standing to lose a wife, mother, daughter, sister, or friend in the coming years unless interventions are made.”
Few diseases reflect global inequities as much as cancer of the cervix. Nearly 90% of 2018 deaths occurred in low and middle-income countries, where the burden of cervical cancer is greatest, because access to public health services is limited and screening and treatment have not been widely implemented.
There is nothing more tragic than suffering and dying from a disease that is preventable through vaccination. The United Nations health agency is recommending vaccination to those between the ages of 9 and 14.
“Eliminating any cancer would have once seemed an impossible dream, but we now have the cost-effective, evidence-based tools to make that dream a reality,” said Dr. Tedros. “But we can only eliminate cervical cancer as a public health problem if we match the power of the tools we have with unrelenting determination to scale up their use globally.”
Prevention of cervical cancer should start early – before girls are exposed to human papillomavirus (HPV). “The vaccine provides up to 95% coverage against cervical cancer,” Dr. Chia Yin Nin, a gynecologic oncologist practicing at Gleneagles Hospital in Singapore, told Business World.
The cervix is part of the female reproductive system located at the junction of the vagina and the uterus (womb). It is often called the neck of the womb. “Generally, all women who have had sexual intercourse are at risk of cervical cancer,” points out the Department of Health (DOH). “However, rare types of cervical cancer can occur even in women who never had any sexual intercourse in their life.”
In recent years, however, there has been overwhelming evidence that HPV causes cancer of the cervix. HPV takes several forms, which are referred to by number. “There are about 100 types of HPV that generally infect people in various parts of the body but there are only 13 types that can cause cancer in the cervix,” wrote Dr. Cecilia Ladines-Llave in a paper presented at the Global Conference on Low-Resource Setting Cervical Cancer Prevention held at the Johns Hopkins University.
The most common causes of cervical cancer are HPV Types 16 and 18. These two types are responsible for 70 percent of cervical cancer around the world. HPV Type 16 also causes oropharyngeal cancer. Condoms do not fully protect against infection because the virus can exist throughout the genital area and around the anus.
“We realize that, although HPV is sexually transmitted, it is not a sexually transmitted disease,” Dr. Nin explained. “It can be acquired through personal contact like fondling, petting and sexual intercourse.”
The following had been established as possible causes of cervical cancer: have had multiple sexual partners, have had sexual partners (regular or casual) who themselves had several sexual partners, have had sexual partner who is infected with HPV, and had first sexual intercourse at a very early age, possibly 15 or 16 years old.
The risk of developing cervical cancer is increased by the following: smoking, long-term use of oral contraceptives, a weakened immune system, and a family history of cancer, especially cervical cancer.
HPV is so prevalent in the community, almost all women can have it. However, there are many forms of HPV, and many do not cause problems. “HPV infections usually clear up without any intervention within a few months after acquisition, and about 90% clear within 2 years,” the UN health agency says. A small proportion of infections with certain types of HPV can persist and progress to cervical cancer.
Dr. Llave, who is the director of Cervical Cancer Prevention Network, was quoted as saying by state-run Philippine News Agency (PNA) that 99.7% of cervical cancers are caused by HPV.
It takes 10 to 30 years of incubation before HPV infection becomes symptomatic. “There are no signs and symptoms about 18% of the time,” Dr. Llave stated. “Most women don’t go to the health centers unless they’re bleeding profusely and they experience too much pain.
For about 20% of the women who are infected with HPV, cervical cancer may develop. “It is only when the cancer develops that you experience the signs like bleeding during intercourse, bleeding between menstrual periods, or bleeding after menopause,” Dr. Nin said. “The patient can also experience other symptoms like back pain, cough and swelling in the abdomen or limbs if the cancer has spread.”
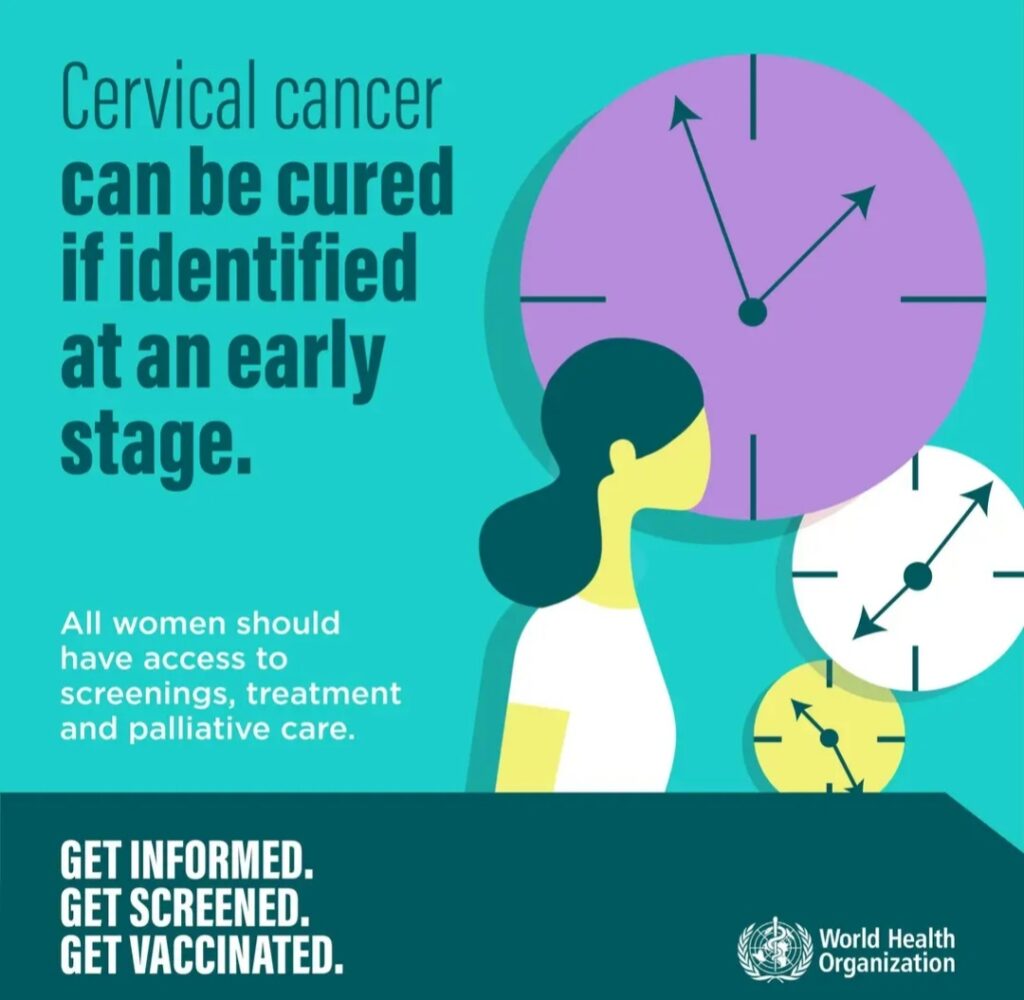
According to Dr. Llave, women diagnosed with stage 1 cervical cancer have 90 percent chance of survival while those diagnosed with stage 3 cervical cancer have 60 percent chance of survival. “Even those at stage 4 still have a 20 percent chance of survival,” she said.
When detected early, cervical cancer, however, is curable. At present, the most reliable and practical way to diagnose cervical cancer early is through Pap smear. Also called Papanicolaou test, it involves collecting cells from the cervix, which are examined under a microscope.
“A woman’s first Pap smear should be done three years after the first vaginal intercourse,” the DOH says. “After that, it should be done every year for 3 years. If the Pap smear test is negative for the consecutive 3 years, then it can be done every two or three years. In unmarried women who never had sexual activity in their life, Pap smear should be done at age 35.”
Aside from Pap smear, there is also the HPV test kit. “It is a swab test similar to the Pap smear,” Dr. Nin said. “The accuracy is so much better than the Pap smear. It is so accurate that you can space out your screening to 3-5 years. For Pap smear, it is recommended that you test once every year because it is quite prone to interpretation error.”
An ounce of prevention is better than a pound of cure, so goes a saying. Currently, there are 3 vaccines protecting against both HPV 16 and 18, which are known to cause at least 70% of cervical cancers. The third vaccine protects against three additional HPV types, which cause a further 20% of cervical cancers.
The WHO reports that clinical trials and post-marketing surveillance have shown that these HPV vaccines are very safe and very effective in preventing infections with HPV. The vaccines, however, cannot treat HPV infection or HPV-associated disease, such as cancer.
HPV vaccines work best if administered prior to exposure to HPV.
Meanwhile, the Philippines wants to eliminate cervical cancer as a public health problem in the country within 7 years. It is only considered eliminated when all countries reach and maintain an incidence rate of less than 4 per 100,000 women.
The global strategy was adopted by the World Health Assembly in 2020. Each country needs to practice three key actions and meet corresponding targets:
· Vaccination: 90% of girls fully vaccinated with the HPV vaccine by the age of 15;
· Screening: 70% of women screened using a high-performance test by the age of 35, and again by the age of 45; and
· Treatment: 90% of women with pre-cancer treated and 90% of women with invasive cancer managed. – ###