By Henrylito D. Tacio
FORMER American Vice-President Dan Quayle never knew what hit him. He was promoting his memoir, Standing Firm, when he experienced severe shortness of breath and had trouble finishing his speeches.
He thought it was just a bad cold and didn’t bother to see a doctor. It was a bad decision. On November 27, 1994, he was brought to the emergency room at the Indiana University Medical Center. The doctor’s diagnosis: “walking pneumonia.”
Quayle, then 47, was sent home and thought it was over. The following day, however, his breathing difficulty worsened and was admitted to the emergency room again. After further tests, doctors re-diagnosed his condition as a “pulmonary embolism” or having a blood clot in his lung.
“You’d be surprised how often a pulmonary embolism is missed, even with most skilled physicians,” Quayle said in a statement following his release. “Misdiagnosis is common. I was lucky…very lucky.”
He was indeed very lucky. In the United States, pulmonary embolism is the third most common cause of death in hospitalized patients, with at least 650,000 cases occurring annually. Autopsy studies have shown that approximately 60 percent of patients who died in the hospital had pulmonary embolism, and the diagnosis was missed in up to 70 percent of the cases.
In other parts of the world, the incidence of pulmonary embolism varies substantially from country to country. Experts claim that “observed variation” is likely due to differences in the accuracy of diagnosis rather than the disease incidence.
“In the 1990’s, it was believed that Filipinos are less susceptible to pulmonary embolism,” says Dr. Willie T. Ong, a cardiologist at the Manila Doctors Hospital. “But recent reports seem to indicate that we are at similar risks.”
What is it?
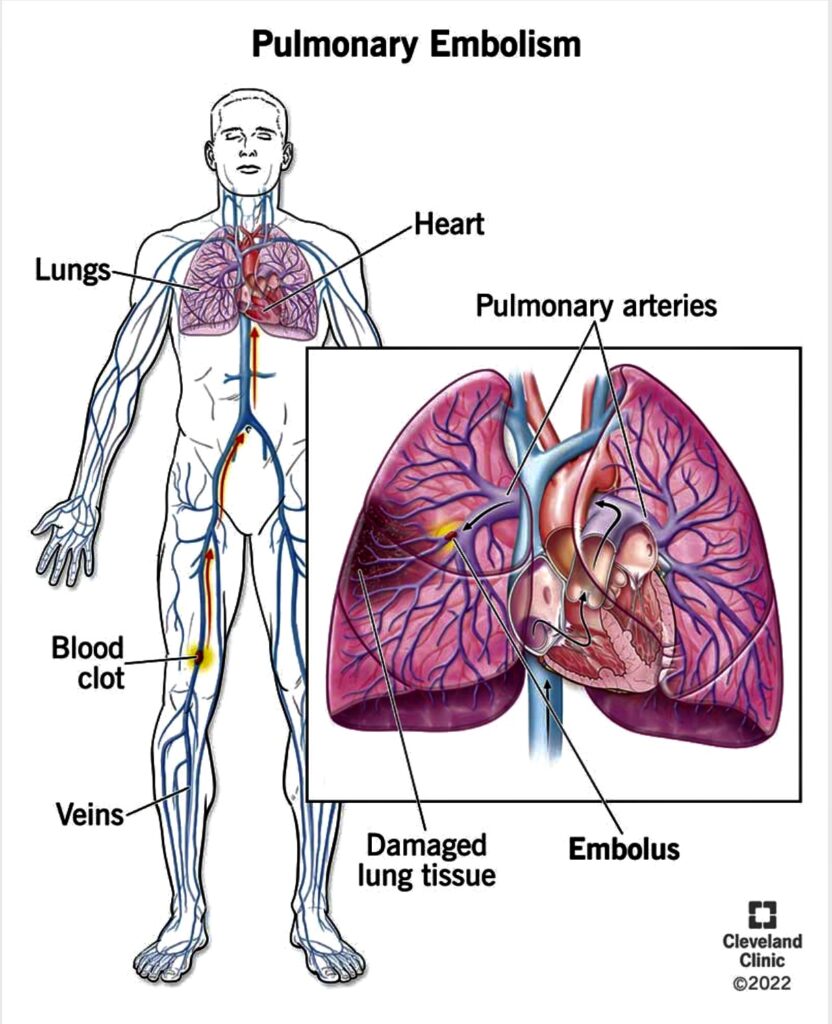
The Minnesota-based Mayo Clinic defines pulmonary embolism as “a condition that occurs when an artery in your lung becomes blocked. In most cases, the blockage is caused by one or more blood clots that travel to your lungs from another part of your body.” Generally, pulmonary embolism is a complication of deep vein thrombosis (DVT).
Most of these blood clots originate in the legs, but they can also form in the arm veins, the right side of the heart or even at the tip of a catheter placed in a vein. In rare instances, other substances, such as a globule of fat, tissue from a tumor or a clump of bacteria, may lodge in the arteries of the lungs.
Signs and symptoms
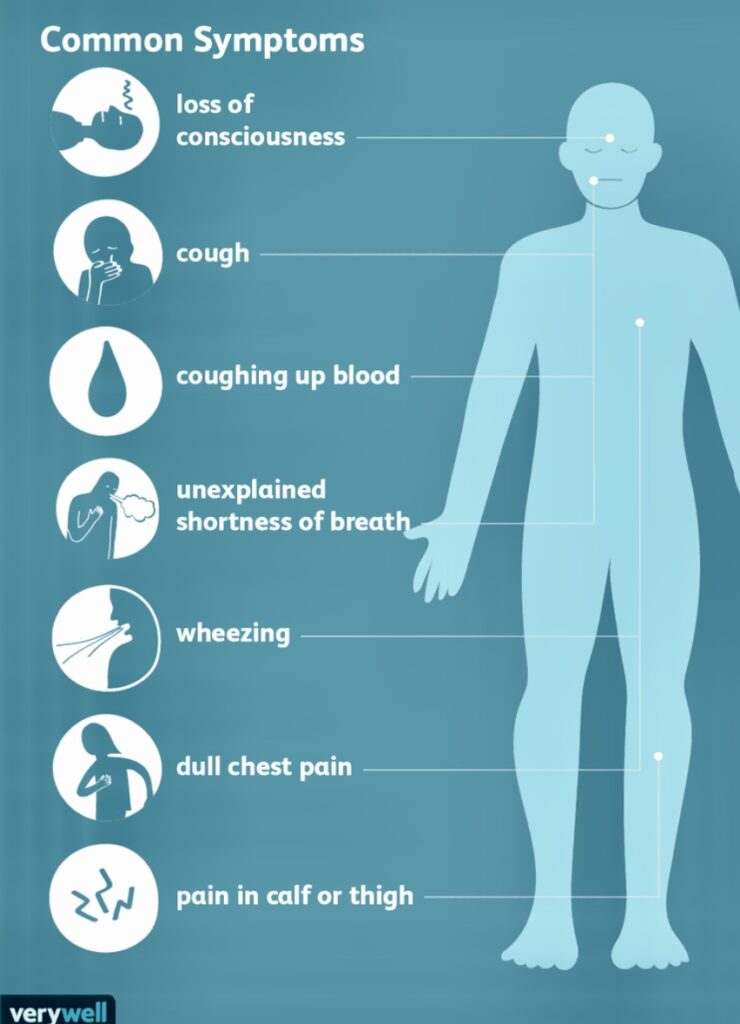
Common signs and symptoms include: sudden shortness of breath, either when you’re active or at rest; chest pain that often mimics a heart attack; a cough that produces bloody or blood-streaked sputum; excessive sweating; rapid heartbeat; and lightheadedness or fainting. Other symptoms, as identified by the Journal of American Medical Association, are as follows: wheezing, clammy or bluish-colored skin, leg swelling, weak pulse, and anxiety.
“Up to 50 percent of all pulmonary embolism cases are unknown – most likely even higher – since most people may not experience any symptoms at all,” says Dr Walter Fister, whose special interest is on public health and works with the Mount Elizabeth Medical Centre in Singapore.
The cause of blood clots in the veins may not be discernible, but many times predisposing are obvious. These conditions include: advanced age, blood clotting disorder (hypercoagulable state), cancer, heart attack, heart failure, irregular heartbeat (atrial fibrillation), major surgery, obesity, paralysis, fracture (pelvis, hip, or leg), prior blood clot, prolonged bed rest or inactivity (such as sitting during a long car or plane trip), stroke, and use of oral contraceptives (especially after age 35 and in someone who smokes). “If you have these risk factors, then you are at increased risk,” Dr. Ong warns.
Hard to diagnose
Pulmonary embolism is hard to diagnose because the symptoms are broad and resemble those of other diseases. “It is often an elusive diagnosis unless the attending physician considers the possibility that the patient is having one,” explains Dr. Arvin Lomugda, a medical internist. “There are predisposing conditions that would make the physician be wary of the possibility because symptoms alone like dyspnea, chest tightness, and tachycardia are nonspecific to the disease.”
Actually, clotting the blood is “nature’s way of trying to prevent bleeding,” says Dr. Rafael Castillo, a cardiologist and chair of the department of medicine of the Manila Sanitarium and Hospital. But when nature’s protective mechanism goes awry, there is a danger of blood clots.
“Blood clots are rare,” the Mayo Clinic assures. “They affect one or two people in every thousand, mainly older people.” Oftentimes, it occurs among people who are undergoing prolonged bed rest or taking long plane or car trips. Such inactivity decreases blood flow in your veins, making clots more likely.
“If a person is just sitting around and not moving, say, during a very long flight, he may risk himself developing pulmonary embolism,” says Dr. Gary Raskob, dean of the college of public health at the University of Oklahoma Health Sciences Center. Such a thing had happened to Dan Quayle. (In France, researchers from the Hospital Pasteur claim that air travelers who sit for more than five hours on planes are more likely to develop blood clots in their legs than non-travelers.)
Pulmonary embolism strikes anyone: young or old, male or female. “There is no sex predilection,” points out Dr Ong. “It depends on the risk factors. More males smoke but females take pills and hormone replacement therapy.” A study done in the United States found significant increases in pulmonary embolism in healthy women taking combined estrogen and progestin.
“About 10 percent of people with pulmonary embolism suffer some lung tissue death (called pulmonary infarction),” explains The Merck Manual of Medical Information. “Sometimes the body breaks up small clots quickly, keeping damage to a minimum. Large clots take much longer to disintegrate, so more damage is done. Large clots may cause sudden death by blocking so much of the lung arteries that the oxygen supply to the body is inadequate to sustain life or by placing an excessive strain on the heart.”
If left untreated, pulmonary embolism is fatal in one in 10 people. Current treatments range from the use of Streptokinase to dissolve the clot to the use of vena caval filters to filter the thromboembolic material towards the lungs, and to invasive thromboendarterectomy.
Doctors generally prescribe a drug called heparin for the first few days after the clot has been diagnosed. After a few days, the patient is then given another drug called warfarin. Both of these drugs thin the blood allowing it to flow more easily around the body and dissolve the clot.
When taking these blood-thinning drugs patients usually have regular blood tests to make sure they are getting the right dose and are not at risk of a hemorrhage.
“The use of heparin should be stopped once the dose of warfarin has stabilized,” reminds Dr. Haizal bin Haron Kamar, associate professor in medicine and cardiology at the University of Malaya in Kuala Lumpur, Malaysia.
“If you think you are suffering from pulmonary embolism, you should immediately see a cardiologist,” suggests Dr Lomugda. “After all, an ounce of prevention is better than a pound of cure.”
The Merck manual said that about half of the people with untreated pulmonary embolism will have another embolism. As many as half of these recurrences may be fatal. Recent studies in the United States have shown that anticoagulant treatment can reduce the rate of recurrence to about one in 20 people; only about one in five of these people will die of pulmonary embolism.
A study done by the National Heart, Lung, and Blood Institute (NHLBI) of the US National Institutes of Health has found that low doses of warfarin prevent recurrence of blood clots. “Our research confirms that low dose warfarin is a safe and effective way to prevent future episodes of these potentially serious blood clotting problems,” said Dr. Claude Lenfant, NHLBI director. – ###
Graphic credits:
1) Pulmonary embolism up close: Victor Jasan. Shutterstock
2) Common symptoms: Verywellhealth.com
3) Pulmonary embolism: Cleveland Clinic