Key Developments from DOH, PhilHealth, and Congress — What Changed, What its implications are, What to Watch
By the H&L Editorial Team
Executive Snapshot
Entering 2026, Philippine health policy is converging around a single narrative: financial risk protection through PhilHealth, zero-balance billing, and stronger primary care, supported by targeted public-health campaigns and disease-specific legislation. The ambition is clear; execution and governance remain the decisive tests.
1. Department of Health (DOH)
What Changed
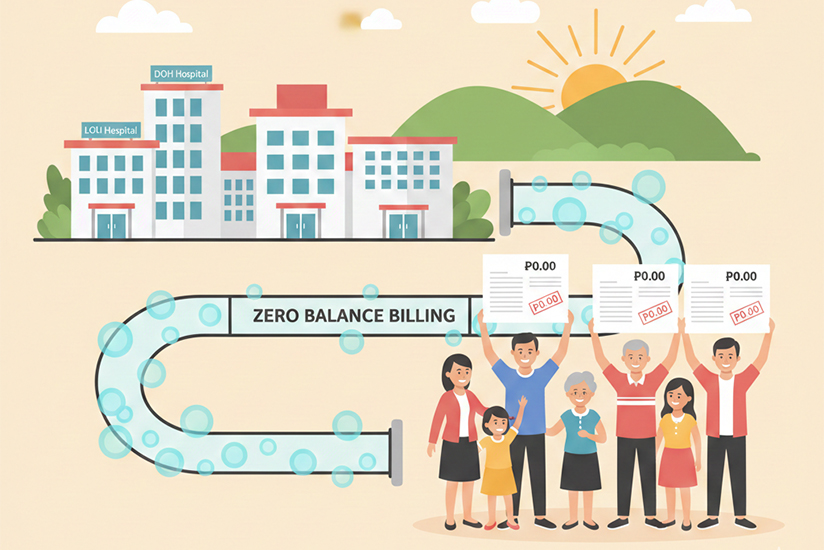
- Expansion of Zero Balance Billing (ZBB) in selected DOH- and LGU-run hospitals.
- Launch of “PinaSiglang 2026,” a year-long healthy-living campaign anchored on 12 simple habits.
- Rollout of a nationwide measles–rubella supplemental immunization campaign, targeting over 10 million children amid rising measles cases.
Implications
- ZBB directly addresses catastrophic health spending—but only if hospital billing practices are strictly enforced.
- Lifestyle nudges like PinaSiglang 2026 are cost-effective population tools, though historically difficult to sustain beyond launch.
- The measles campaign is a high-stakes operational test of DOH’s logistics, LGU coordination, and vaccine confidence rebuilding post-pandemic.
Risks & Red Flags
- ZBB leakage through “informal” charges or misclassification of services.
- Campaign fatigue for lifestyle programs without LGU ownership.
- Uneven immunization coverage in geographically isolated and disadvantaged areas (GIDAs).
2. PhilHealth
What Changed
- One-time waiver or reduction of interest penalties on unpaid employer contributions from 2013–2024, with incentives for immediate settlement.
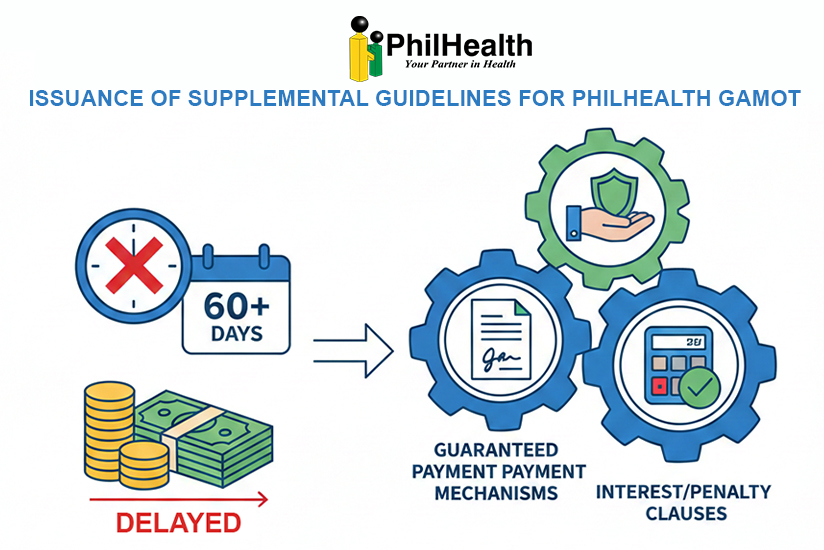
- Issuance of supplemental guidelines for PhilHealth GAMOT, clarifying safeguards when reimbursements are delayed beyond 60 days.
- Continued rollout of YAKAP Primary Care Benefits, reinforcing outpatient consultations, diagnostics, and selected medicines.
Implications
- The contribution penalty waiver is both a collections reset and a coverage-stabilization strategy.
- GAMOT guidelines implicitly acknowledge a chronic system issue: delayed payments threaten provider participation.
- YAKAP signals a long-term pivot from hospital-centric care to preventive, outpatient-first UHC.
Risks & Red Flags
- Moral hazard if penalty waivers become routine.
- Provider attrition from GAMOT if payment delays persist.
- Fragmented YAKAP implementation across regions and IT systems.
3. Congress and Senate
What Changed
- Ratification of the 2026 national budget with increased health allocations, including PhilHealth subsidies and ZBB support.
- Senate approval on third reading of the Comprehensive Lupus Prevention Act, establishing a national framework for a chronic autoimmune disease.
- Continued congressional emphasis on medical assistance programs and indigent care.

Implications
- Budget signals are strongly pro-UHC—but history shows that appropriations do not guarantee outcomes.
- Disease-specific laws reflect a maturing health policy agenda, shifting from episodic aid to structured national programs.
Risks & Red Flags
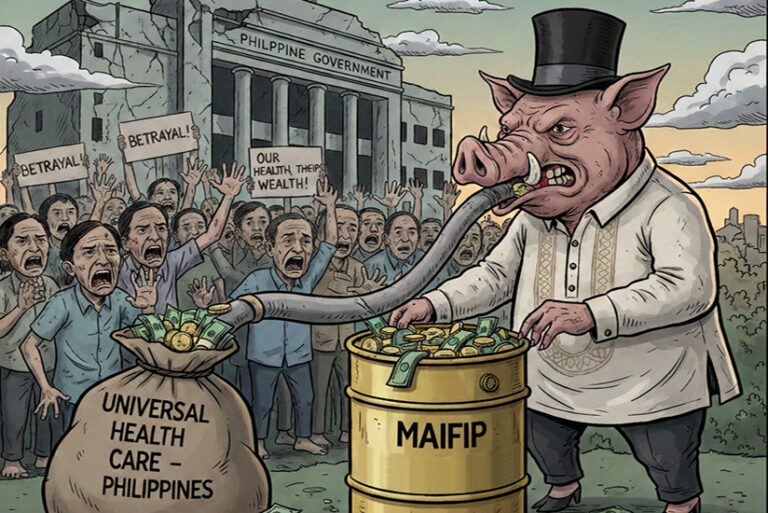
- Weak safeguards in large assistance funds invite leakage and politicization.
- Disease-specific laws risk fragmentation if not harmonized with PhilHealth benefit design and DOH service delivery.
Cross-Cutting Assessment
The Direction Is Right.
2026 policy choices favor:
- Reduced out-of-pocket spending
- Stronger primary care
- Preventive public health
The Vulnerability Is Execution.
Persistent risks include:
- Delayed PhilHealth payments
- Inconsistent hospital billing discipline
- Weak monitoring and accountability
What to Watch Closely in 2026
- Actual ZBB compliance audits and patient complaint data
- PhilHealth claims turnaround time, especially for GAMOT
- YAKAP provider enrollment and patient utilization rates
- Measles immunization coverage by region, not just national averages
- Budget execution versus budget approval
Bottom Line
The Philippines is not short on health policies or funding signals. The defining question for 2026 is simpler—and harder:
Can the system finally deliver timely payments, honest billing, and consistent primary care at scale?