Diabetes is no longer a slow, distant threat—it is quietly reshaping Filipino lives long before symptoms appear. Today, millions live with undiagnosed diabetes or prediabetes, discovering the disease only when complications have already taken hold. This cover story lays out an evidence-based, Philippines-ready blueprint to stop diabetes before it steals years of healthy life.
By Rafael R. Castillo, MD
On paper, diabetes looks like a slow disease—numbers inching upward, complications appearing “later,” symptoms that many people can ignore for years. In real Filipino life, it moves faster: the tricycle driver who can’t feel his feet, the lola whose blurry vision is dismissed as “age,” the middle-aged office worker who discovers a sky-high blood sugar only after a wound refuses to heal.
The tragedy is not that diabetes is mysterious. The tragedy is that it is often silent, predictable, and detectable—yet missed.

Diabetes is one health crisis where the science is clear and the tools are already in our hands. With smarter screening, earlier treatment, and systematic identification of high-risk Filipinos, the Philippines can bend the diabetes curve—saving lives, protecting families from catastrophic costs, and preventing complications that never needed to happen.
The Philippines is already carrying a heavy burden: the International Diabetes Federation (IDF) estimates about 4.7 million Filipino adults (20–79) living with diabetes in 2024, with an adult prevalence of around 7.5%. And unless the country changes its approach, the IDF projects the number could rise to approximately 8.6 million by 2050. Globally, diabetes has become so widespread that the IDF estimates 1 in 9 adults live with it—and over 4 in 10 don’t know they have it.
That “don’t know” is the doorway where the Philippines can win—because diabetes is one of the few major chronic diseases where early detection + early action can dramatically reduce kidney failure, stroke, heart attack, amputations, blindness, and catastrophic out-of-pocket costs.
What follows is an evidence-based, practical blueprint: Find it earlier. Treat it earlier. Protect organs earlier.
The Missing Years: Why diabetes is often diagnosed late

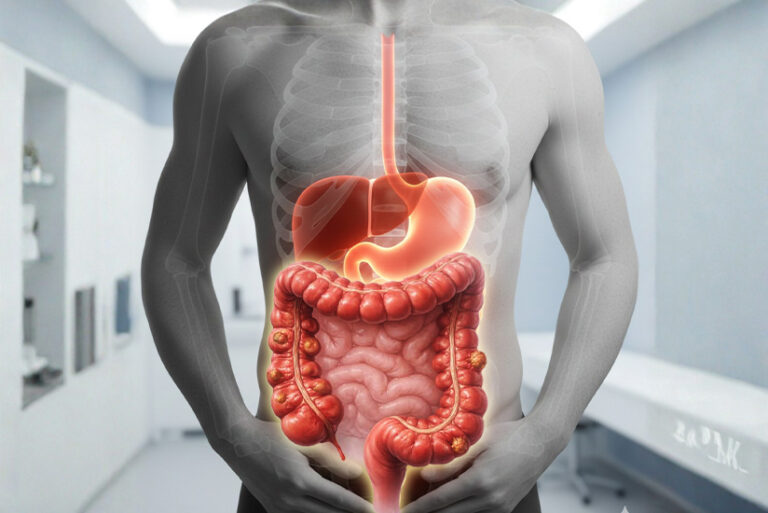
Type 2 diabetes does not usually begin with drama. It begins with insulin resistance and rising blood sugar that may not yet cause symptoms. Many people function normally while damage quietly accumulates—especially in blood vessels, kidneys, nerves, and eyes.
Late diagnosis happens for familiar reasons:
- No symptoms early on, or symptoms are misread as “pagod,” “stress,” “age,” or “mahilig lang sa tubig.”
- Screening is inconsistent—often done only when someone feels sick.
- Risk is underestimated in people who don’t “look” unhealthy.
- Access gaps: time, cost, distance, or lack of a regular primary care home.
The fix is not to blame patients. It is to redesign the system so that screening becomes as routine as renewing a driver’s license—especially for those at highest risk.
Step 1: Diagnose earlier—with clear, standard tests
Diabetes is diagnosed using established laboratory thresholds. The American Diabetes Association (ADA) recognizes diagnosis based on any of the following (with confirmation when appropriate): A1C, fasting plasma glucose, 2-hour glucose on an oral glucose tolerance test, or random glucose with classic symptoms.
For A1C specifically, ADA lists:
- Diabetes: A1C ≥ 6.5%
- Prediabetes: A1C 5.7–6.4%
- Normal: A1C < 5.7%
Why is this important? A1C is convenient (no fasting), but it can be costlier and less available in some areas. Fasting blood sugar is cheaper and widely used. The best approach is not “one test for all,” but a tiered strategy: use what’s available—then confirm and act.

A practical Philippines-ready screening ladder
Level 1 (community / workplace / primary care):
- Risk assessment + waist/weight + blood pressure
- Fasting blood sugar when feasible
Level 2 (confirm and classify):
- A1C (especially if fasting is a barrier)
- OGTT for selected cases where diagnosis is uncertain or high-risk (e.g., pregnancy protocols are separate)
Step 2: Find the high-risk—before they become “patients”
If the country waits for symptoms, it will always be late. The smarter goal is to identify:
- Undiagnosed diabetes
- Prediabetes
- High-risk states that predict diabetes and heart/kidney disease
Who should be prioritized for screening?
A high-yield approach is to prioritize adults with:
- Overweight/central obesity (waistline matters in Asians)
- Family history of diabetes
- Hypertension or abnormal lipids
- History of gestational diabetes (or large baby)
- Sedentary lifestyle
- Fatty liver suspicion
- Signs of insulin resistance (e.g., acanthosis nigricans)
This is not “medical gatekeeping.” It is public health triage: screen where the probability is highest.
Step 3: Use the system we already have—PhilHealth Konsulta as a diabetes “front door”

One underused opportunity is PhilHealth’s Konsulta package, which includes laboratory tests relevant to diabetes detection, including fasting blood sugar, OGTT, and HbA1c (among others).
That means the Philippines already has a policy pathway that can be strengthened into a national habit:
- If every Konsulta-accredited primary care team treats diabetes risk screening as a default—especially for high-risk adults—late diagnosis can drop.
The question is no longer “Do we have a mechanism?” The question is “Will we scale and standardize it so it works the same way in every barangay and city?”
Step 4: Treat earlier—because early treatment prevents expensive tragedy
“Treatment” is often imagined as pills. But early diabetes care is actually a bundle:
- Lifestyle therapy (food quality, movement, sleep, stress)
- Evidence-based medications when indicated
- Blood pressure and lipid control
- Smoking cessation
- Kidney and eye protection
- Vaccination updates and foot care education
Modern standards emphasize that diabetes is not just about sugar; it’s about preventing organ damage. The ADA Standards of Care are updated annually and include strategies for diagnosis, prevention, and treatment.
A practical “First 100 Days after Diagnosis” playbook
If the Philippines wants fewer dialysis chairs filled by preventable diabetes, the first 100 days after diagnosis should be standardized:

- Confirm diagnosis and baseline labs
- Assess cardiovascular and kidney risk
- Set realistic targets (not perfection—progress)
- Start lifestyle coaching that is culturally Filipino (rice realities included)
- Start medication when needed (guided by clinician and patient context)
- Schedule follow-up with urgency (not “balik ka in 6 months”)
Step 5: Make prevention visible—Prediabetes is the “save point”
Prediabetes is not a label for shame; it is a window for reversal. Globally, a large share of adults live in that gray zone—high enough risk to matter, early enough to change.
A national diabetes strategy must treat prediabetes as a priority population:
- Not every prediabetic person needs medication.
- But every prediabetic person needs a plan, follow-up, and support.
The public message should be simple:
“Hindi ka pa diabetic—pero puwede pang pigilan.”
Step 6: Policy levers that actually move the needle
1. Keep strengthening the sweetened beverage tax—and link it to prevention programs

The Philippines’ TRAIN Law included an excise tax on sweetened beverages, with rates described in policy analyses (e.g., PHP 6/L and a higher rate for certain sweeteners). Evidence suggests taxation and related policies can reduce sugar-sweetened beverage intake and encourage reformulation—especially when paired with labeling and advertising guardrails.
Best practice: Taxes work better when the public sees where the money goes—like school water stations, barangay exercise spaces, and subsidized screening.
2. Standardize primary care protocols for NCDs
The Philippines has long pursued essential NCD intervention protocols (e.g., PhilPEN) aimed at integrated screening and early management. The opportunity now is execution discipline:
- same screening triggers
- same follow-up schedule
- same minimum lab bundle
- same referral thresholds
3. Build a national “diabetes detection engine”

Think of it like contact tracing—except for risk:
- workplaces (BPOs, factories)
- schools/parents (family-based screening)
- churches and civic groups
- pharmacies
- LGU days (e.g., “Know Your Numbers” weekends)
What success looks like by the end of 2026
Not a miracle. A measurable shift:
- More diagnosis at earlier stage (higher proportion detected before complications)
- Higher screening coverage among high-risk adults
- More people with prediabetes enrolled in structured lifestyle programs
- Better control of blood pressure and kidney risk markers in diabetics
- Fewer “first presentation = dialysis” stories
A final word: Diabetes is a test of national organization
Diabetes is not defeated by slogans. It is defeated by systems:
- routine screening
- fast follow-up
- consistent primary care
- affordable labs and medicines
- culturally realistic lifestyle support
- protection of heart, brain, kidney, eyes, and feet—early
The Philippines can bend the curve. But it must stop treating diabetes as a late-stage complication problem—and start treating it as a detection and early-action problem.
Because the most expensive diabetes patient is not the one who needs medicine today.
It is the one who needed a simple test—two years ago.
“The most expensive diabetes patient is not the one who needs medicine today—it is the one who needed a simple blood sugar test two years ago.”
References
- International Diabetes Federation (IDF). Diabetes in The Philippines (2024): prevalence and estimates.
- International Diabetes Federation (IDF). Diabetes facts and figures (IDF Diabetes Atlas 2025): global prevalence and undiagnosed proportion.
- American Diabetes Association (ADA). Diagnosis & Tests (A1C thresholds for normal/prediabetes/diabetes).
- ElSayed NA, et al. ADA Standards of Care 2025—Diagnosis and Classification of Diabetes. Diabetes Care.
- American Diabetes Association (ADA). Standards of Care in Diabetes (professional guidelines hub; includes 2026 access point).
- PhilHealth. Konsulta Package Circular (2024) and lab inclusions (FBS, OGTT, HbA1c).
- Onagan FCC, et al. Development of a sweetened beverage tax, Philippines (TRAIN Law policy analysis). BMJ Global Health / PubMed Central.
- Philippine Journal of Science (DOST). Monitoring sugar-sweetened beverage consumption related to TRAIN Law (policy input).
- WHO. Noncommunicable diseases: global burden overview (context for NCD strategy framing).
WHO / Philippines. PhilPEN document (essential NCD interventions approach—integrated screening/management framework).